Understanding Fascia Tightness: What It Means & How to Support It
- Joy Zazzera

- Feb 18, 2024
- 4 min read
Updated: Aug 23
Common Misconceptions About Fascia Tightness
You may have heard that your fascia is “tight,” “wound up,” or “needs to be released.” These phrases are common in wellness spaces—but are they accurate? What does it actually mean when we feel stiff, restricted, or like we need to “stretch something out”?
As a Yoga Medicine® Therapeutic Specialist and massage therapist, I work every day with adults who feel bound up, stiff, or limited in movement—especially those with joint replacements or long-term tension patterns. And what science tells us about fascia might surprise you.
Let’s explore what’s really going on beneath the surface—and how therapeutic movement, stretching, and self-massage can help.

Myth #1: “Fascia Can Be Tight”
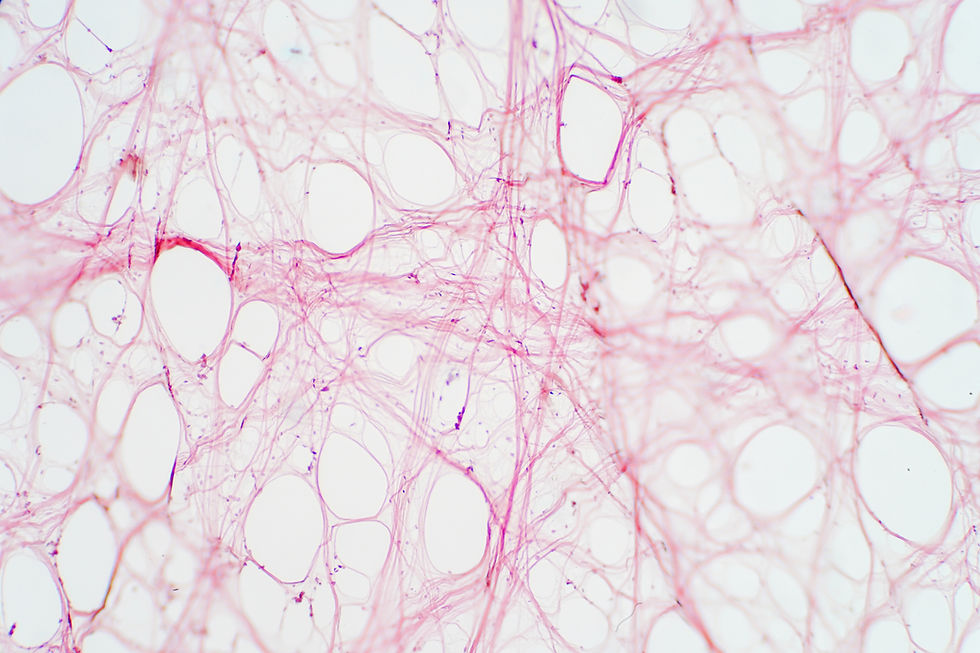
Fascia is a type of connective tissue that wraps around and weaves through your muscles, nerves, and organs. It includes both dense (like tendons and ligaments) and loose forms—most notably, areolar connective tissue, which plays a key role in mobility.
So can fascia be “tight”? In very specific medical cases—fascial tightness can be an accurate diagnosis. But most of the time, what we describe as tightness is more about nervous system tone and tissue resistance, not literal fascial contraction.
Fascia and The Nervous System: What You’re Probably Feeling Is… Sensation
The feeling of being “tight” is largely a neurological experience, not a mechanical one. This is especially true with areolar connective tissue, where collagen fibers are held together by weaker intermolecular bonds. These bonds can reorganize—but they don’t contract like muscle.
So when you feel stiff or restricted, you’re likely sensing:
Increased nervous system tone (your body’s protective reflexes)
Local tissue resistance
A lack of movement variability
Possibly even fear or anticipation of pain
None of these are signs of permanent damage—but they do deserve attention.
Frozen Shoulder: A Rare but Real Fascial Contracture
One exception is adhesive capsulitis, or frozen shoulder—a true case of fascial fibrosis and contracture. In these rare instances, fascia becomes pathologically thickened and shortened, leading to real structural limitations. But even here, research shows that movement and therapeutic input make a difference, especially when done consistently.
Myth #2: “You Can Release Fascia Instantly”
So, can fascia be released? The short answer: not in the way many people think.
The term “release” is vague. Fascia doesn’t melt, break apart, or instantly lengthen under pressure. But change still happens, especially through:
Nervous system response (the fast-acting kind of "release")
Passive stretching (which encourages reorganization, not lengthening)
Consistent input over time (which improves local tissue health and mobility)
Myth #3: “”Self-Massage Breaks Up Fascia"
Massage and self-massage can absolutely influence how you move and feel—but mostly by calming your nervous system and helping tissues reorganize, not by “breaking up” fascia.
Connective Tissue & The Relaxation Response: Why Areolar Connective Tissue Responds Best
The most adaptable fascial tissue is areolar CT, found in the interstitial spaces between your muscles and skin.
It’s rich in hydration, vascular flow, and innervation—which means it responds beautifully to:
Gentle, sustained stretching
Breath-based movement
Self-massage techniques (like rolling or compression)
These practices improve organization of the fascial layers, enliven hydration, increase blood flow and support the body’s relaxation response, which is key for mobility and healing.
Myth #4: “Stretching Lengthens Fascia Permanently
Stretching Helps—But It's Not a Fix-All.
Stretching can help reorganize collagen fibers in areolar fascia, but it won’t change dense fascia (like tendons or ligaments). And the effects are temporary unless practiced consistently. That’s why it’s more accurate to say we’re influencing fascia—not fixing or releasing it.
What we’re really doing is:
Reducing perceived tightness
Improving movement variability
Enhancing local blood flow
Supporting nervous system adaptation
A Note on Perspective and Growth
I’ve been studying and teaching about fascia since 2018—not just from textbooks, trainings and course work or even cadaver dissections, but through lived experience. As someone living with bilateral knee replacements and idiopathic (of unknown origin) scar tissue buildup, I understand firsthand how connective tissue issues can impact movement, healing, and quality of life.
My perspective is both clinical and deeply personal. And because I continue to train in anatomy, fascia science, and nervous system research, my understanding—and my teaching—continues to evolve. You may notice that my older blog posts or class content reflect different ways of explaining or thinking about fascia. That’s intentional.
I believe it’s essential to update what we teach as science advances. My goal is not just to offer practices that feel good, but to offer education that reflects the most accurate, current insights—while remaining compassionate and practical for real bodies, real limitations, and real lives.
Lasting Change Requires Consistent Input
Early changes from stretching or self-massage are mostly neurological—they come quickly, and fade just as fast. But over time, with regular, mindful input, tissues can adapt. Fibroblasts (fascial cells) may reorganize, reduce tension signals, and improve glide between tissue layers.
That’s why repetition and routine matter. It’s not about “fixing” tightness—it’s about building a relationship with your body over time.
The Bottom Line: You’re Not Broken—You’re Adaptable
You don’t need to be more flexible to feel better. What you need is to understand what’s really happening in your tissues—and how to support them with therapeutic practices that nurture, rather than force, your body toward ease.
Whether you're recovering from surgery, managing movement challenge or chronic tension, or just feeling stiff from daily life, you can improve how you move and feel—not by “releasing” fascia, but by inviting your body into gentle, consistent reorganization.
Want more clarity on fascia, movement, and nervous system health?
Subscribe to my [Yoga with Joy’s Newsletter] for science-backed, therapeutic yoga tools designed for adults with movement limitations, joint replacements, common movement restrictions, and chronic stress.







Comments