Gentle Yoga for Low Back Pain Relief
- Joy Zazzera

- Apr 27, 2024
- 5 min read
Updated: Aug 23
Therapeutic Tools for Real-Life Spine Support
Low back pain affects up to 80% of people at some point in their lives. And yet, no two experiences of pain are exactly the same. One person may feel stiffness or deep achiness; another may deal with nerve pain, instability, or postural strain. What’s important to understand is this: even when imaging shows degeneration, bulging discs, or misalignment, pain is not always directly tied to structure. And even when there are no structural issues at all, pain can still be very real.
As someone trained in yoga therapeutics, massage therapy, and pain science—and as someone who’s lived with joint replacements and tissue damage—I’ve seen firsthand how healing requires more than just “fixing” the body. It’s about support, nervous system regulation, and learning how to move in ways that feel safe, stable, and empowering.
This blog post offers insight into how yoga therapeutics can help with common low back conditions and how to adapt practice for your real body, right now.
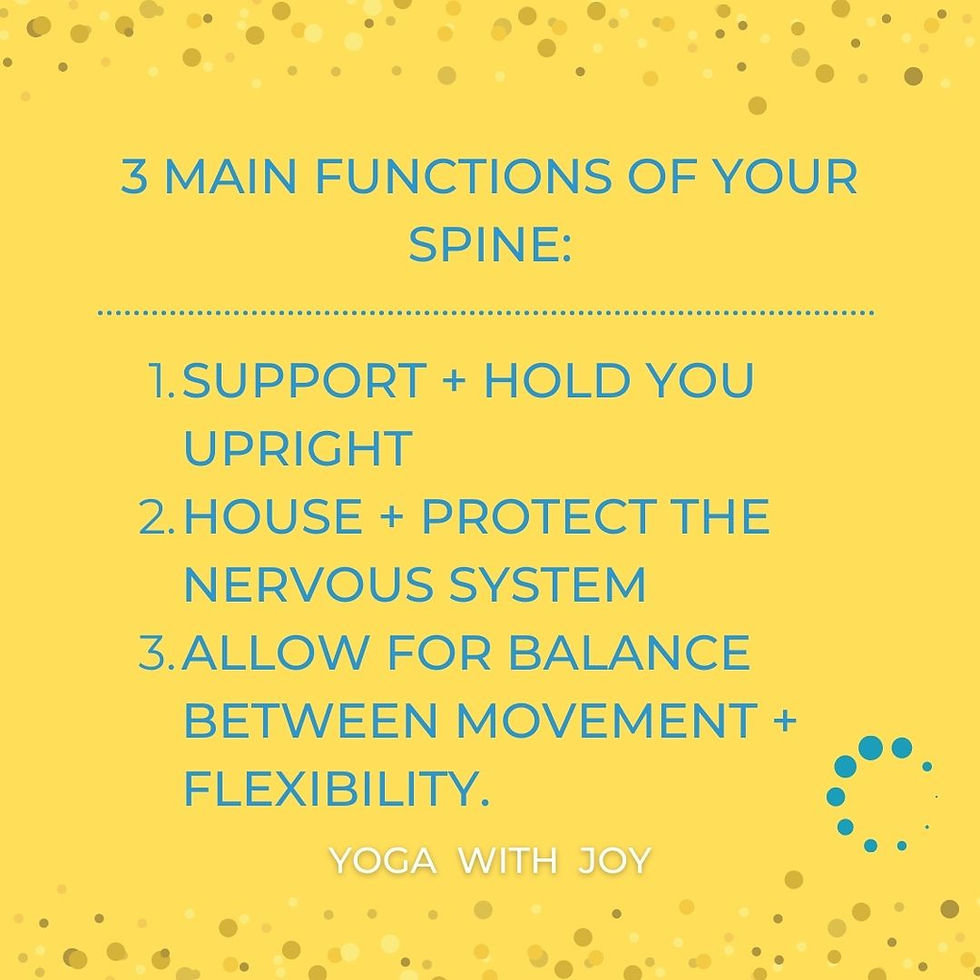
Understanding the Spine: Not Just Bones and Discs
Your lumbar spine is responsible for a wide range of movement—flexion, extension, lateral flexion—with very limited rotation. But what many people don’t realize is that low back pain often arises from a combination of factors including:
Poor muscular support (especially multifidus and deep core muscles)
Thoracolumbar fascia dysfunction
Postural imbalance
Trigger points in muscles like quadratus lumborum (QL), glutes, and psoas (the hip flexors)
Diminished mobility in surrounding regions (thoracic spine, hips, diaphragm)
It’s not always about one big injury. It’s often a pattern of stress, instability, and compensation over time.
Gentle Yoga for Low Back Pain for Common Low Back Conditions
Before we look at specific spinal conditions, it’s important to understand how gentle yoga taught through a therapeutic lens differs from general exercise or traditional yoga. It’s not about achieving advanced poses or pushing through discomfort. Instead, therapeutic yoga focuses on purposeful movement, nervous system regulation, and restoring function over time—using techniques that are informed by both science and sensitivity.
Whether you're working with me through a structured program for common low back conditions or in a 1-on-1 setting customized for your unique challenges, the approach is always therapeutic and intentional. In personalized 1-1 sessions, I begin by observing how you move—your posture, breath, habits, and areas of compensation—often through Zoom-based assessment. In structured programs, the sequences are thoughtfully designed to address the most common pain patterns and mobility limitations, while still offering safe, progressive support.
In yoga therapeutics, we work with both the mechanical and subjective aspects of pain:
You may have no structural issue on a scan, but still feel a lot of pain.
Or you may have clear structural changes (like disc degeneration), but no pain at all.
This is why pain is personal—and why our work must be, too.
Rather than focus only on what’s tight or weak, we look at the entire support system: deep stabilizers, breath mechanics, compensatory patterns, and emotional context. We use tools like supine positioning, small stabilizing movements, supported transitions, and self-myofascial release to gently rebuild function.
Most importantly, we don’t rush. Stabilization takes time—often 5 to 8 weeks of consistent, gentle practice to see results. But with the right guidance and patience, yoga can become one of the safest, most empowering ways to move through and beyond low back pain.
Here’s a look at how yoga can support some of the most common spinal issues:
1. Disc Herniation and Sciatica
Disc issues often involve nerve compression (usually at L4–S3), which can cause pain, numbness, or tingling down the leg. Sitting too long can aggravate the psoas, which increases lumbar pressure.
Yoga Therapeutics Focus:
Supine postures to reduce load on the spine
Gentle core engagement (transverse abdominus, multifidus) to support the spine
Avoid deep forward folds; explore small, controlled movement
Use sciatic nerve flossing and movement in unloaded positions
2. Facet Joint Pain & Osteoarthritis
Pain during rotation or extension may point to facet joint irritation or rib subluxation. While arthritis and disc degeneration sound alarming, they’re not always painful.
Yoga Therapeutics Focus:
Balanced support to reduce wear and tear
Explore postures that do not provoke extension or rotation
Improve mobility above and below the site of discomfort
Incorporate myofascial release (self-massage) and slow, progressive challenge
3. Stenosis
Narrowing of the spinal canal can increase nerve sensitivity. Forward folding can feel relieving.
Gentle Yoga for Low Back Pain Therapeutics Focus:
Gentle flexion postures
Avoid strong backbends
Slow roll-ups (unlike disc issues which may find this aggravating)
Emphasis on spinal elongation and core activation
4. Spondylolysis / Spondylolisthesis
These conditions involve a vertebral defect or slippage, often exacerbated by hyperextension.
Yoga Therapeutics Focus:
Strengthen tranverse abdominus (TVA) and multifidus
Limit back-bending and shearing motions
Avoid high-load positions like deep squats or unsupported twists
5. Postural Conditions
From hyperlordosis to flat back and sway back, postural habits influence spinal mechanics.
Yoga Therapeutics Focus:
Teach pelvic alignment and neutral spine awareness
Use tools like yoga straps or broomstick assessments
Focus on glute and deep core engagement (TVA, pelvic floor)
Offer permission to move without “perfect” posture
Trigger Points & Muscle Dysfunction
Chronic back discomfort often arises from referred pain patterns in surrounding soft tissue:
QL: can mimic disc pain and is aggravated by asymmetrical load (e.g., heavy bags on one side)
Gluteus medius/minimus: common referral into the sacroiliac (SI) joint and down the leg
Psoas: tightness increases disc pressure; aggravated by prolonged sitting
Rectus abdominis: tension can pull on the lumbar spine and limit range of motion
Therapeutic Approach:Release techniques like myofascial release (self-massage), passive range of motion, and breath-based core work can help bring relief while rebuilding stability.

A Therapeutic Path Forward: Stability Over Time
Relief doesn’t come from pushing harder—it comes from moving smarter. Especially during acute flare-ups, yoga should emphasize:
Unloading the spine (supine postures, bolstered support)
Creating simple, progressive movement patterns
Teaching students how to use their legs and core to shift load
Encouraging language that empowers rather than creates fear
Building core strength—especially in the transverse abdominis, multifidus, and glutes—takes time. Expect 5–8 weeks of consistent practice before seeing meaningful shifts in support and sensation.
A Final Word: The Subjective Side of Pain
Pain is deeply personal. Your MRI or X-ray doesn’t always explain what you’re feeling. There can be significant mechanical issues with no pain—or significant pain with no visible issue.
As yoga students, our job isn’t to “fix” ourselves but to become more curious, compassionate, and consistent in how we move. When we focus on stability, breath, and sensation—not just shape—we start to reclaim a sense of trust in our own spine.







Comments